Bita's Journey

• Developed the first national telemedicine platform and telemedicine services in the country
• Established the Telemedicine Research Center at Beheshti University of Medical Sciences
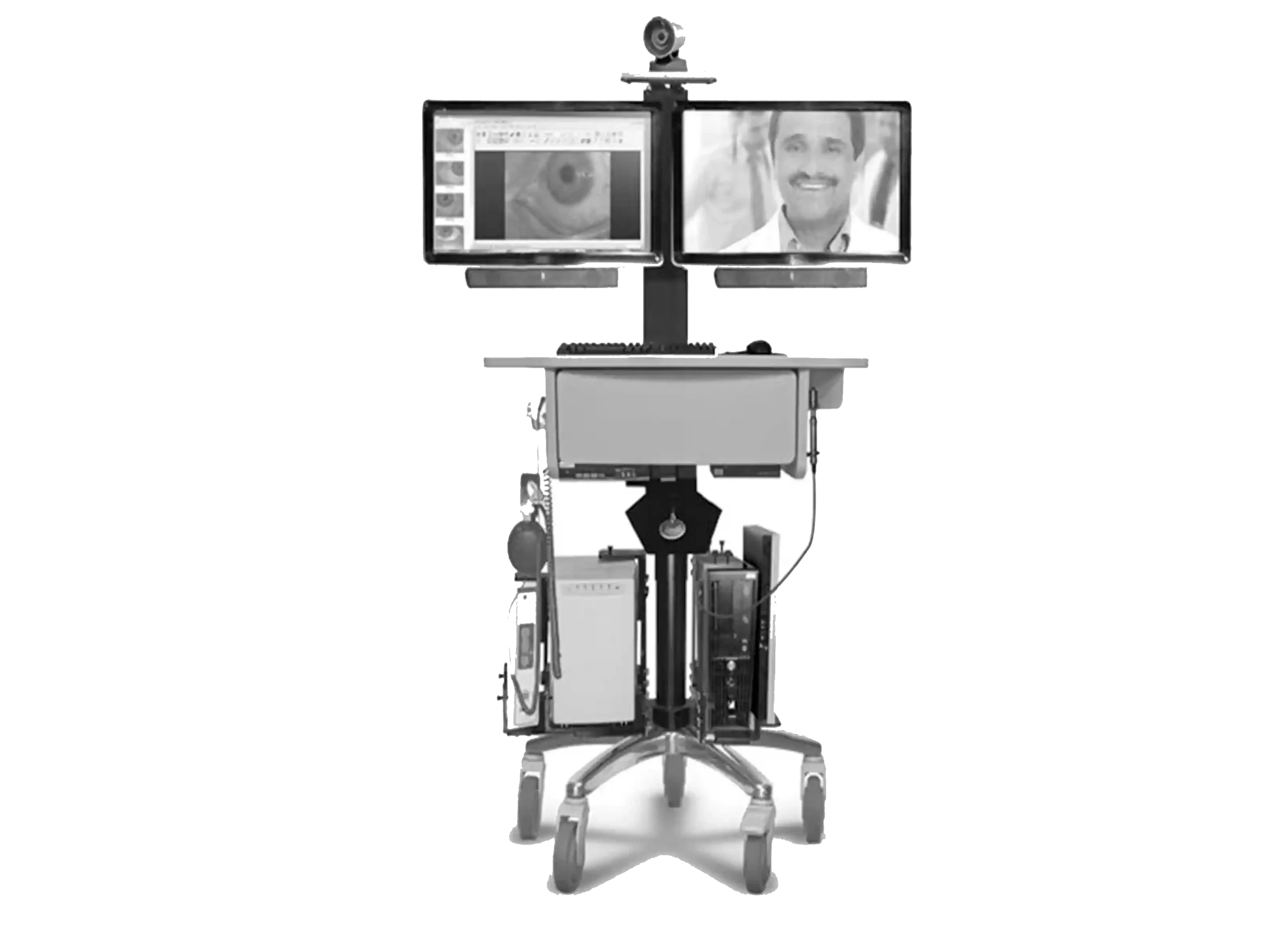
• Developed Telemedicine Electronic Medical Record Software and Telemedicine Hardware to connect satellite hospitals to the hub hospital
• Built the network infrastructure to be able to provide telemedicine services remotely to two (2) satellite hospitals and connect them to the hub hospital
• Launched Tele-ICU, Tele-Cardiology, Tele-Pulmonary, and Tele-ER clinical services with eight (8) physician attendees and multiple residents in the Satellite locations
• Created provider training for all four (4) locations to utilize the telemedicine software and hardware
• Developed and refined a PACS system at the University and trained three (3) radiologists to use it
• Expanded Tele-ICU to two (2) new facilities across Tehran, boosting patient reach same day, and evaluated telemedicine expansion opportunities in the region
• Developed and evaluated telemedicine hardware and software, enhancing care for patients treated via ambulance in remote areas, leading to a new standard of delivery care model with improvement in response times
• Conducted comparative analysis of patient lung and heart exams using the Telemedicine digital stethoscope versus traditional clinical exams across four (4) facilities and discovered an improvement in quality of care for Tele-cardiology patients

• Wrote and received grants, developed, implemented, and maintained the infrastructure for 20 service lines in VA hospitals and ambulatory clinics telemedicine programs
• Developed service contracts, policies, and procedures that became the national standard, leading to a 20% improvement in consistency and compliance across telemedicine programs
• Exceeded all program expectations and received excellent ratings from 95% of patients
• Launched a Tele-EP Program (cardiac electrophysiology) in 2014 and had eight (8) remote clinics managing numerous complicated patient cases each week
• Reduced wait times from 12 months to three months and saved patients 50K miles of travel in cardiac electrophysiology services
• Provided $1M of hospital-bound care for just $218K during the first year with Tele-EP
• Doubled Tele-EP program for just $466K in the second year and tripled the program to eight clinics in 2016 for a cost of only $609K for the equivalent of $3M of in-hospital treatment
• Established Tele-Sleep program in 2012 with 12 nurses in eight remote clinics providing care to 60 patients weekly, with 6K patients receiving care between 2012 and 2015
• Cut wait times from 18 months to three months and eliminated 900K miles of patient travel to receive Sleep Medicine Care
• Reduced the cost of a sleep evaluation from $2K to $500 for program participants
• Provided $4.5M equivalent in hospital-bound care for just $670K total over three (3) years in Tele-Sleep Services
• Received accolades for the program, which was used as a model for nine other VA hospitals and was permanently funded with improved access to sleep care nationwide
• Established 17 additional revenue-generating programs including Home Telehealth, Tele-PAP, Tele-Insomnia, CVT-Home, Tele-HPBS, Tele-Epilepsy, Tele-Genetic, Tele-HIV Clinic, Tele-Liver Clinic, Tele-Oncology, Tele-Hematology, Tele-Poly Trauma, Tele-Rehab Amputee, Tele-Wound, Tele-Pre-Op, Tele-Post Op and Tele-Mental Health

• Developed a physician-driven, enterprise-wide, scalable Virtual Care Services offering across the CommonSpirit Health system of 142 hospitals and 1200 clinics in 21 states, providing 2.3M virtual visits
• Chaired the national physician and clinical team experience for Common Spirit Health for 8600 physicians
• Acted as the key stakeholder of the National Patient Experience Virtual Health Committee for seven years
• Served as the key adviser on all matters related to Virtual Care and continually evaluated and developed growth plans for Virtual Care programs, resulting in a 300% expansion in services
• Defined the value proposition for Virtual Care: improve access, clinical outcomes, care experience, and affordability, leading to a 25% increase in patient access, a 23% improvement in clinical outcomes
• Created a national in-patient telehealth survey with Press Ganey, gathering critical data that led to a 15% improvement in patient satisfaction
• Streamlined Tele-Specialty services for endocrinology, cardiology, multiple sclerosis, pulmonology, palliative care, mental health, geriatrics, electrophysiology, neurosurgery, and neurology, expanding patient access to specialized care and improving outcomes by 32.1%
• Onboarded and trained 1200 physicians in California in one week and provided 200K+ virtual visits in six weeks
• Charged with leading the National COVID Home monitoring service from Hospital to home and in clinics, resulting in an 86% reduction in hospital readmissions
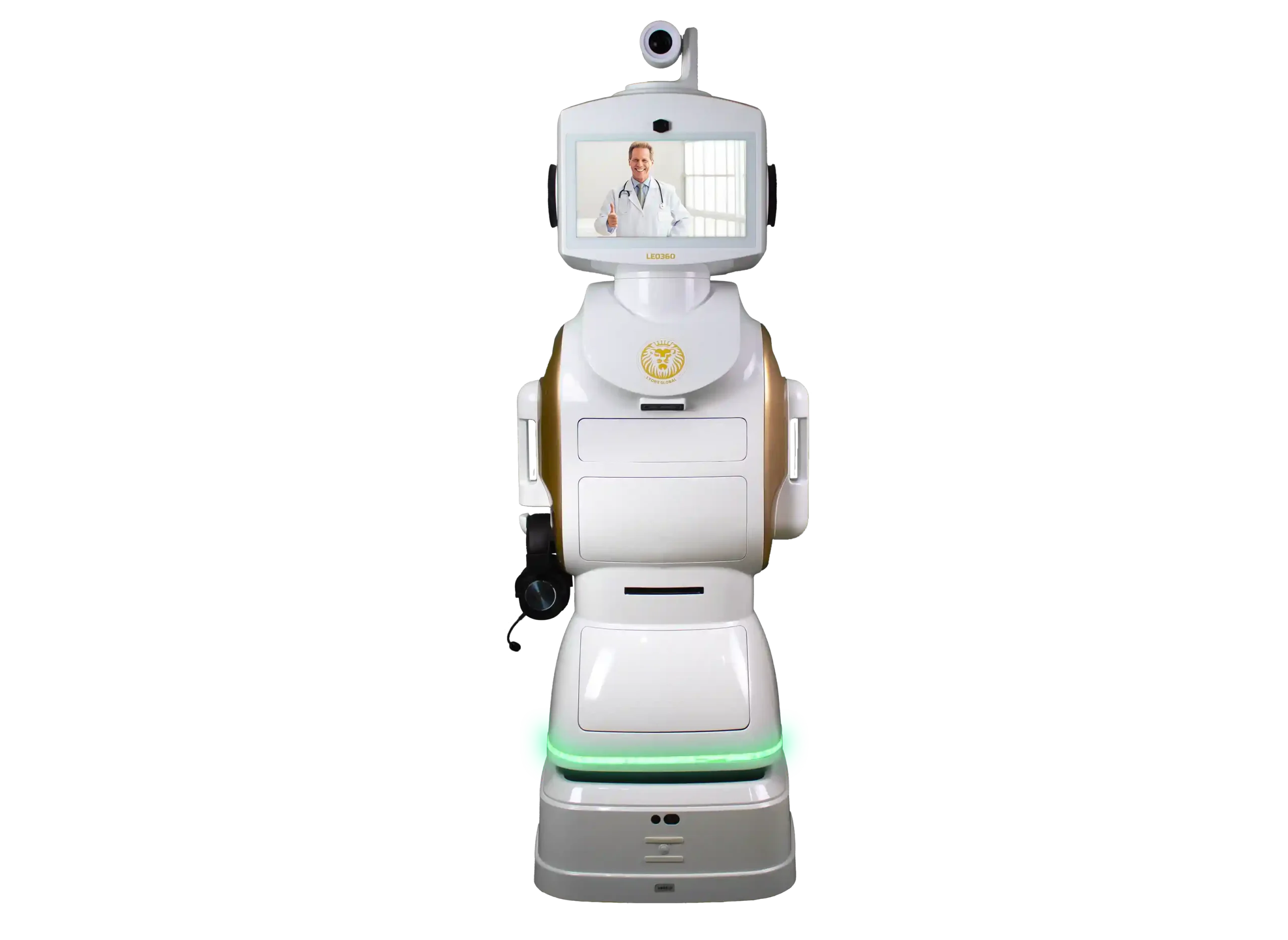
• Reconfigured a tele-clinic robot in collaboration with InTouch Health, which cut the price by 43% and improved the quality of interactions between clinicians and patients
• Delivered Remote patient monitoring of 500 asthma patients, achieving zero (0) readmissions; remote monitoring of high-risk chronic disease patients, reducing hospitalization by 73% and ER visits by 69%
• Provided enterprise-wide Virtual Care policy, scheduling, and billing, analytic outcomes, and ROI graphs
From 2006 to the LEO360® Breakthrough 2024