Using remote patient monitoring to improve care and cut costs
July 2021 | Medical Group Management Association
COVID-19 has been a major accelerator for digital transformation in healthcare. Organizations that embraced this transformation have continued to thrive during the pandemic. Among those is the Mercy Medical Group (MMG), a multispecialty group practicing throughout the greater Sacramento, Calif., area.
MMG partnered with Dignity Health to implement an innovative remote patient monitoring (RPM) program, using RPM for monitoring COVID-positive patients and patients with multiple chronic diseases. MMG is now piloting RPM for post-operative patients. Early results have been impressive:
• RPM-enrolled COVID positive patients showed a 76% reduction in hospitalizations
• RPM-enrolled patients with chronic diseases showed a 38% reduction in hospitalizations and 28% reduction in ER visits.
• RPM-enrolled post-operative patients showed a 30% reduction in length of stay, with patient satisfaction at 97%.
RPM programs track patient health outside a traditional clinical setting. RPM refers to the specific technology used to electroni- cally transmit information between patients and clinicians. Monitoring programs can collect a wide range of health data such as vital signs, weight, blood pressure, blood sugar, blood oxygen levels, heart rate and electrocardiograms. RPM offers the advantage of remotely caring for patients with mobility issues. Healthcare providers can also continu- ously monitor patients and detect illness in real time, which can prevent worsening of illnesses and untimely deaths. From a patient quality perspective, it offers options for non-invasive medical interventions and the ability to be cared for at home. For payers, it reduces high costs associated with ER visits and preventable hospitalizations.’
Providers use RPM for patients of all ages, although senior patients drive the best return on investment (ROI) because of the high incidence of multiple chronic diseases. A KLAS Research report found 38% of healthcare organizations running RPM programs focused on chronic. care management reported reduced admissions, while 17% cited cost reductions. Some of the most frequently targeted conditions include:
• Care transitions: post-hospital, post-surgical
• Cardiovascular: heart failure, hypertension, post-cardiac surgeries
• Endocrine: diabetes
• Mental health: anxiety, bipolar disorder, de- pression, substance abuse
• Orthopedic: post-surgical for hip or knee
• Renal: end-stage renal disease (ESRD), chronic kidney disease (CKD)
• Respiratory: asthma, chronic obstructive pulmonary disease (COPD), COVID-19, pneumonia.
Challenges
There are several challenges when designing an RPM system. First is the decision to use a contact or contactless method. Then there is the selection of sensors, processing algorithm and communication network. Another critical factor is the accuracy and reliability of the tools being used. Finally, the medical community needs to approve of RPM, and patients need to consent to participate.
MMG’s RPM PROGRAM
MMG is a multispecialty medical group compris- ing approximately 485 physicians and clinicians caring for more than 250,000 patients across the greater Sacramento, Calif., region. The group has been in operation for 75 years and has repeatedly earned “Elite Status” from America’s Physician Groups’ Standard of Excellence program. Almost one-third of MMG’s agreements are based on
value-based payment models. MMG partnered with Dignity Health to establish the Office for Virtual Innovation to identify opportunities to engage patients and care for them in their home environments. One of their innovations is the RPM program in collaboration with Medtronic.
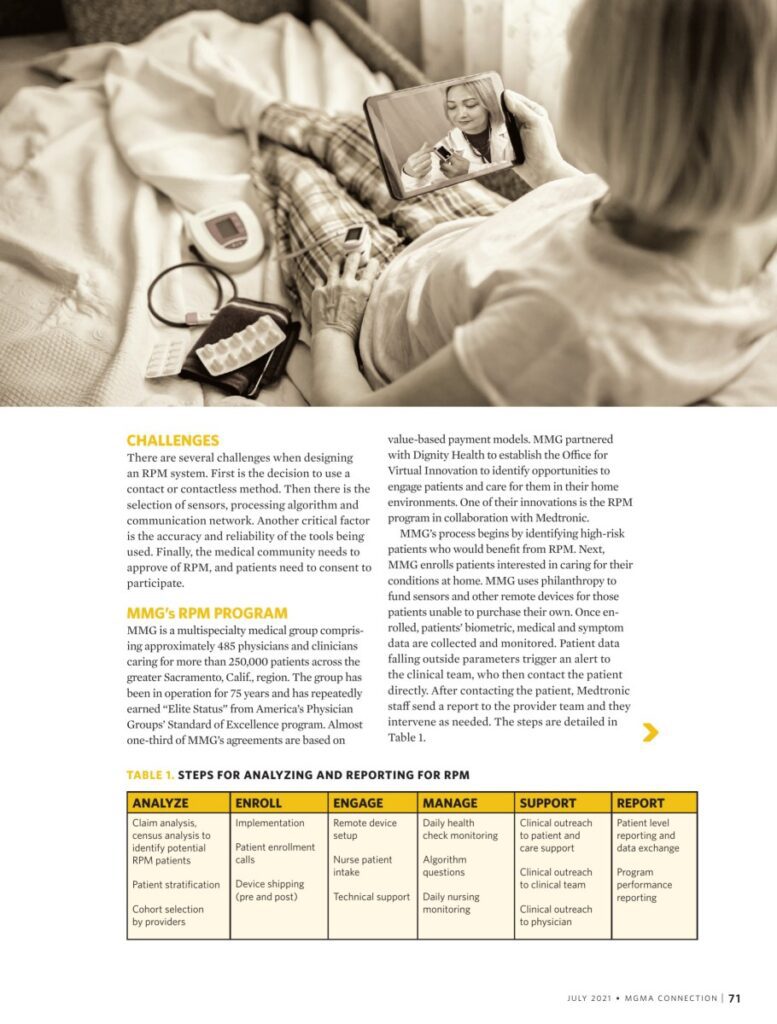
MMG’s process begins by identifying high-risk patients who would benefit from RPM. Next, MMG enrolls patients interested in caring for their conditions at home. MMG uses philanthropy to fund sensors and other remote devices for those patients unable to purchase their own. Once en- rolled, patients’ biometric, medical and symptom data are collected and monitored. Patient data falling outside parameters trigger an alert to the clinical team, who then contact the patient directly. After contacting the patient, Medtronic staff send a report to the provider team and they intervene as needed. The steps are detailed in Table 1.
The program and associated workflows spe- cifically incorporate evidence-based medicine guidelines and patient information that assists with developing ongoing self-management skills. The team also work hard to provide patients feed- back about their progress toward treatment goals and act as patient advocates to encourage patient and healthcare professional communication.
SUCCESSES
MMG has used RPM for three separate pro- grams. In 2017, MMG began a small pilot that included nine patients with congestive heart failure. Prior to enrollment, these patients had multiple presentations to the hospital. Since enrollment, patients have shown 38% reduc- tion in hospitalizations and 28% reduction in ER visits. In 2020, the group used RPM to track 225 patients who tested positive for COVID-19 to monitor for worsening symptoms. Although these patients have had higher rates of virtual visits, they have shown a 76% reduction in hospi- talizations compared to other COVID-19 patients not enrolled in RPM. MMG is using RPM to manage post-operative patients undergoing colon and bowel surgery. To date, MMG has tracked 10 patients with 10 hospital days saved, noting a 30% reduction in length of stay when compared to other patients undergoing the same procedures.
HOW RPM IS COMPENSATED
Implementing RPM often is a strategy to reduce care costs as part of alternative payment models. However, fee-for-service payments still com- prise an average of 70.8% of practice revenue.3 Organizations wanting to implement RPM with limited managed care agreements can cap- ture charges through coding. The five primary Medicare RPM codes include 99091, 99453, 99454, 99457 and 99458. In 2019, CMS initially targeted RPM as services rendered for patients with chronic conditions. CMS waived this restriction during the COVID-19 public health emergency (PHE), allowing practitioners to fur- nish RPM for patients with acute conditions, as well as patients with chronic conditions; how- ever, CMS will probably not extend the waiver beyond the expiration of the PHE.*
To bill for services, patients must opt into RPM. In addition, the device must be supplied for at least 16 days and must meet the Food and Drug Administration’s (FDA) definition of
a medical device. A physician can monitor the data or assign the task to staff.
CONCLUSION
MMG’s innovative RPM program has helped bend the cost curve and improve patient out- comes. Insider Intelligence estimates 30 million U.S. patients (or 11.2% of the population) will use RPM tools by 2024, marking 28.2% growth from 23.4 million patients in 2020. As RPM becomes more commonplace in the industry, healthcare organizations should develop imple- mentation strategies to embrace this model of care delivery to keep pace with more progres- sive players in the market.
Notes
Peter Valenzuela, chief medical officer, Mercy Medical Group
Christine Braid, virtual care physician lead and medical director, ambulatory telehealth, Dignity Health
Bita Farhadpour, virtual care administrative lead and director, ambulatory telehealth, Dignity Health
1. Malasinghe LP, Ramzan N, Dahal K. “Remote patient monitoring: a comprehensive study.” J Ambient Intell Human Comput 10, 57-76 (2019).
2. Sharp B, Buckley C. Remote Patient Monitoring 2018: High Potential in a Shifting Landscape. KLAS Research. Oct. 2, 2018.
3. Rama A. “Policy Research Perspectives: Payment and Delivery in 2016: The Prevalence of Medical Homes, Accountable Care Organizations, and Payment Methods Reported by Physicians.” American Medical Association. 2019.
4. Wein EH, Ferrante TB, Goodman RB, Lacktman NM. “2021 Medicare Remote Patient Monitoring FAQs: CMS Issues Final Rule.” National Law Review. Dec. 7, 2020.
5. Nunn K. “Remote patient monitoring: Building a new outpatient revenue stream.” MGMA. April 25, 2020.
6. Dolan S. “The technology, devices, and benefits of remote patient monitoring in the healthcare industry.” Business Insider. March 10, 2021.